Superior Management, Data, Collections, Transparency and Follow up
Superior Management, Data, Collections, Transparency and Follow up

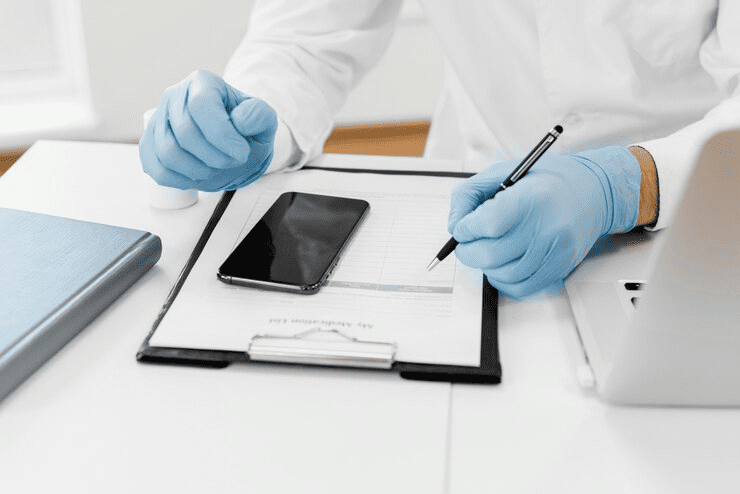
Schedule a Billing Analysis Phone Consultation

Free Accounts Receivable Review

Schedule a Free Medical Billing Consultation

Schedule a Billing Analysis Phone Consultation

Free Accounts Receivable Review